Introduction
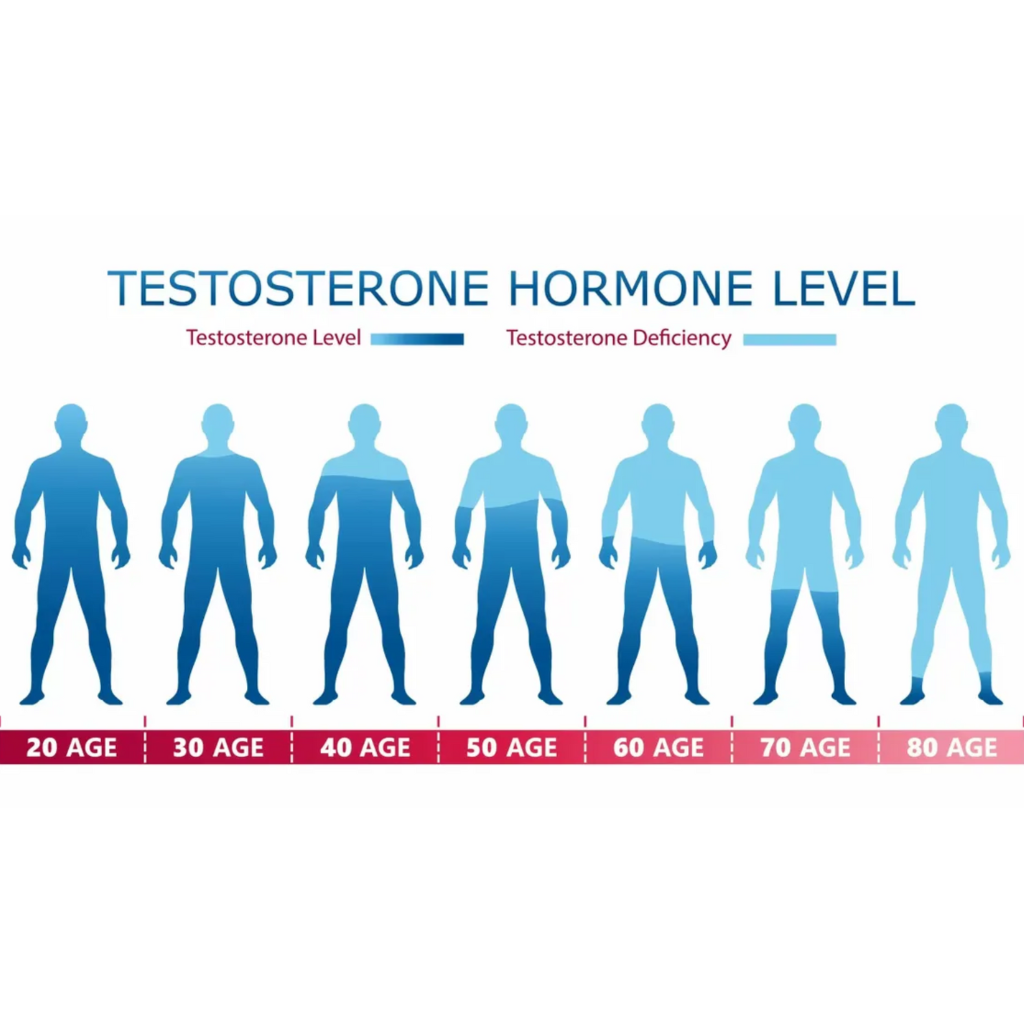
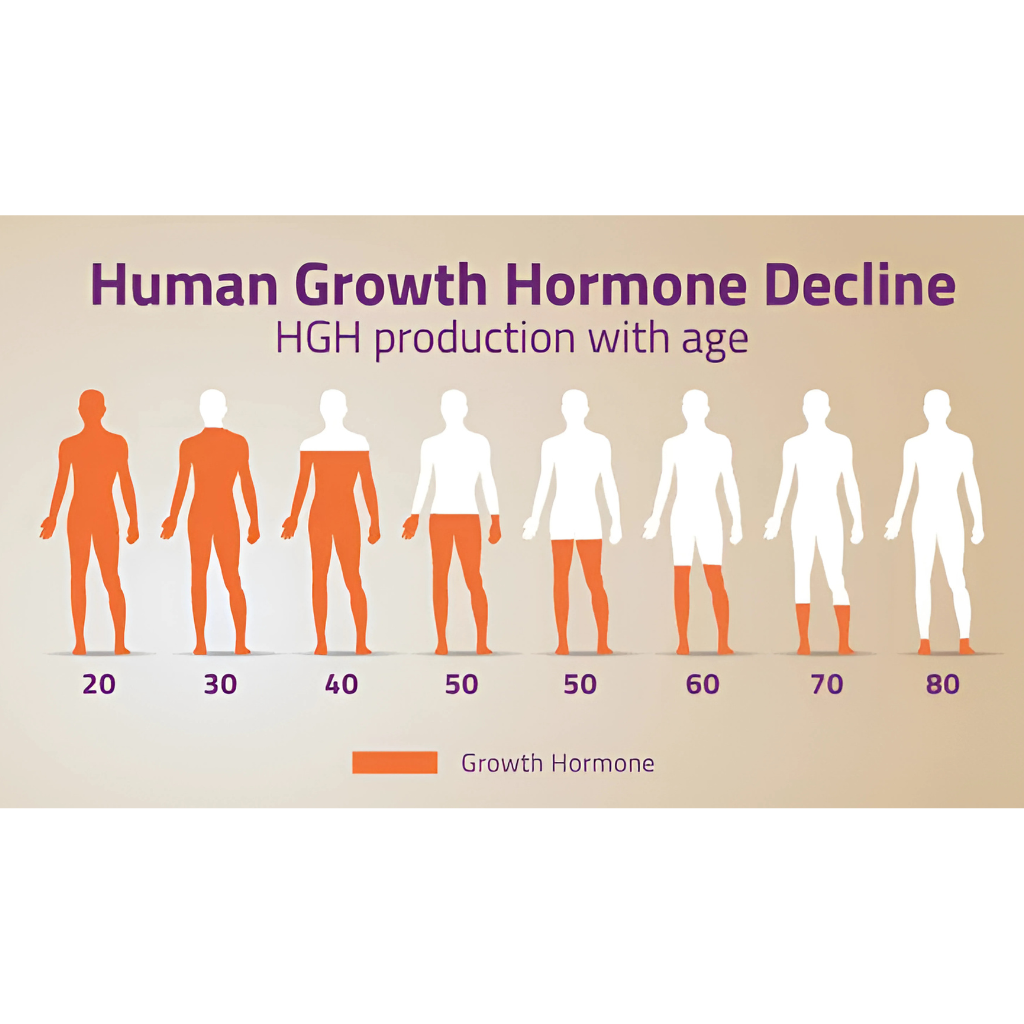
Testosterone is a hormone that is central to the identity make up and daily functions of human beings; as it not only determines permanent characteristics such as facial features during developmental phase, but also determines on a day-to-day the functional activity level of several organ systems such as your brain. After The age of 37 come off mails naturally have a decline of 1% of testosterone levels in their body due to a decrease in production and release. Consequently, a cluster of symptoms emerge when the testosterone levels fall too low, which are commonly ignored due to a lack of knowledge amongst men and peers regarding healthy aging versus rapid deterioration of health. Testosterone replacement therapy is a medical treatment designed to restore testosterone levels to a healthy range and alleviate those symptoms. We are seeing more and more cases of pathologic low testosterone, almost at epidemic levels, due to various environmental factors that are only just starting to be discovered as inciting factors of chronic illness; including seed oils, endocrine disrupting chemicals, an artificial dies in ultra processed foods. In this particular article we will explain what testosterone replacement therapy is come out who might benefit from it and how the treatment is administered through various options.
What qualifies as “low testosterone”?
The American Urological Association defines low testosterone (also called hypogonadism) as a total serum testosterone level below 300 ng/dL. It is important to note that there is controversy and emerging debate regarding using this static baseline level demarcation, rather than an updated age adjusted level in combination with clinical symptoms to make the diagnosis of hypogonadism. The original studies which this number is based off of are more than 50 years old and based off of a different population and characteristics and haven't been updated since then. Common signs include reduced sex drive, erectile dysfunction, decreased muscle mass and strength, loss of armpit or pubic hair, depressed mood and diminished energy. Risk factors include obesity, poorly managed type 2 diabetes and chronic illnesses. Because these symptoms overlap with normal aging or other medical conditions, men should have their testosterone checked via blood test and undergo a thorough evaluation. [1] Using an online clinical quiz, is usually a great step in figuring out if you might have symptoms of low T and hypogonadism.
How TRT works
TRT delivers testosterone into the body through various routes. Options include intramuscular injections, transdermal gels or patches, oral capsules and implantable pellets. Injections provide a measured dose based on a frequency of every one to two weeks. Topical gels or patches absorb testosterone steadily through the skin; and carries the risks of More difficult titration of medication due to unpredictable and volatile absorption rates through the skin. Transdermal application also carries the risk of transference meaning that if somebody else, Such as your wife or kids, comes in contact with the area of skin that you have medication applied that medication can be transferred onto them just like rubbing off sweat onto someone else which would lead to mistreatment. Pellets implanted under the skin can last several months, although are never used in the US as they are known to unsafe from the standpoint of carrying an increased risk of complications such as bleeding, infections, subtherapeutic, discomfort and retained foreign body in skin. Your doctor will help determine which method suits your lifestyle and medical history.
Who is a candidate for TRT?
TRT is appropriate for men who have both symptoms of low testosterone and a laboratory confirmation of low levels. It is not a fountain of youth or a performance enhancer for healthy men. Candidates often include men with primary testicular failure (due to aging, injury or genetic conditions) and men with secondary hypogonadism caused by pituitary or hypothalamic disorders. Obese men or those with poorly controlled diabetes might also benefit, but it’s important to address underlying conditions simultaneously. [2-3]
Benefits of TRT
Clinical studies report that restoring testosterone to the normal range can improve sexual function, mood, energy and muscle mass, and can reduce body fat. Many patients also had improvements in mental health and characteristics such as overall motivation, ambition, general competitiveness and overall well-being. Many of these studies have been able to be reproduced and replicated proving the high level of evidence throughout the world. The strongest literature comes from patients with testicular cancer who have decreased levels of testosterone pathologically and then are treated with testosterone replacement therapy to monitor their effects. Individual results as with any medication will vary depending on adherence to therapy, personalization of protocol, lifestyle factors including diet exercise and sleep. [4-7]
Risks and monitoring
TRT is generally safe when properly monitored and managed, but it can raise red blood cell counts, alter cholesterol levels and affect fertility. Red blood cell counts elevate as the body ramps up production of healthy tissues throughout the body although this can become pathologic if the hematocrit (% concentration of hemoglobin red blood cells) becomes very high; this is problematic as against blood can cause accidents such as strokes, blood clotting disorders and pulmonary embolus. Men should undergo regular blood tests to assess hemoglobin/hematocrit, liver function, lipid profile and prostate‑specific antigen (PSA), Especially if over the age of 40. Those with prostate cancer, breast cancer or severe heart failure should avoid TRT. Discuss potential risks with a healthcare professional before starting therapy. [8]
Conclusion and next steps
Testosterone replacement therapy can transform quality of life for men suffering from symptoms of hypogonadism. The first step is an honest conversation with a healthcare provider and a simple blood test. In general having a patient tested and treated through the conventional outpatient medical pathway in the US health system takes approximately 1-2 months on average.
If you have insurance: schedule an appointment with your primary care physician who may or may not order the blood test for you. The other option is that the primary care physician will refer your care out to a specialist such as an endocrinologist. You will have to schedule an appointment with the endocrinologist and be evaluated at which point the physician may or may not order a testosterone level for you based on your presenting symptoms and physical findings. If the specialist orders a testosterone level check you will then go to your nearest phlebotomy and lab processing service such as lab quest or Quest Diagnostics to have your blood drawn and said to the lab for analysis. After one week of processing your physician who ordered the blood test will get a copy of your results and you will follow up with that physician for another visit to discuss your lab findings. On the follow up visit you may or may not be prescribed testosterone replacement therapy based on your presenting symptoms and lab findings.
If you do not have insurance - the process you will follow will be similar to the above except you will have to pay in cash for the clinic visits as well as having your labs drawn.
The modern medicine approach to testosterone replacement therapy involves clinical intake forms online, telehealth visits, at-home testing through mail, home delivery of medications and refills; all at a fraction of the cost and time of traditional therapy.
References
- Cleveland Clinic. Male Hypogonadism (Low Testosterone). This resource defines low testosterone as under 300 ng/dL and lists symptoms such as reduced sex drive, erectile dysfunction, loss of hair, depressed mood and decreased muscle and endurance my.clevelandclinic.org.
- Testosterone Therapy in Men With Hypogonadism: An Endocrine Society Clinical Practice Guideline. Bhasin S, Brito JP, Cunningham GR, et al. The Journal of Clinical Endocrinology and Metabolism. 2018;103(5):1715-1744. doi:10.1210/jc.2018-00229.
- Testosterone Treatment in Adult Men With Age-Related Low Testosterone: A Clinical Guideline From the American College of Physicians. Qaseem A, Horwitch CA, Vijan S, et al. Annals of Internal Medicine. 2020;172(2):126-133. doi:10.7326/M19-0882.
- Efficacy and Safety of Testosterone Treatment in Men: An Evidence Report for a Clinical Practice Guideline by the American College of Physicians. Diem SJ, Greer NL, MacDonald R, et al. Annals of Internal Medicine. 2020;172(2):105-118. doi:10.7326/M19-0830.
- EMAS Position Statement: Testosterone Replacement Therapy in Older Men. Kanakis GA, Pofi R, Goulis DG, et al. Maturitas. 2023;178:107854. doi:10.1016/j.maturitas.2023.107854.
- The Efficacy and Adverse Events of Testosterone Replacement Therapy in Hypogonadal Men: A Systematic Review and Meta-Analysis of Randomized, Placebo-Controlled Trials. Ponce OJ, Spencer-Bonilla G, Alvarez-Villalobos N, et al. The Journal of Clinical Endocrinology and Metabolism. 2018;:4939466. doi:10.1210/jc.2018-00404.
- Testosterone Replacement in Young Male Cancer Survivors: A 6-Month Double-Blind Randomised Placebo-Controlled Trial. Walsh JS, Marshall H, Smith IL, et al. PLoS Medicine. 2019;16(11):e1002960. doi:10.1371/journal.pmed.1002960.
- Secondary Polycythemia in Men Receiving Testosterone Therapy Increases Risk of Major Adverse Cardiovascular Events and Venous Thromboembolism in the First Year of Therapy. Ory J, Nackeeran S, Balaji NC, Hare JM, Ramasamy AR. The Journal of Urology. 2022;207(6):1295-1301. doi:10.1097/JU.0000000000002437.